The first part of this posting tells how a U.S. Army medical board, headed by Walter Reed, confirmed that the transmission of yellow fever requires a mosquito vector. The second part tells the story of the yellow fever vaccine developed by Max Theiler.
Bearing in mind the enormous benefit to mankind of the polio vaccines developed by Jonas Salk and Albert Sabin (1), and that Maurice Hilleman developed nearly 40 vaccines, including those for measles, mumps, and rubella (2), it would appear remarkable that Theiler was the only one of these four individuals to be recognized by the Nobel committee. In fact, Theiler’s 1951 Nobel award was the only one ever given for a vaccine! In any case, while Theiler’s vaccine was a major step forward in the fight against yellow fever, it came after a perhaps more dramatic episode in the struggle against that malady. But first, we begin with some background.
Yellow fever was another of mankind’s great scourges. Indeed, it was once the most feared infectious disease in the United States. And, while we might want to say that science has “conquered” yellow fever, that statement would not be entirely accurate. Unlike polio and measles, which have nearly been eradicated by the vaccines against them, that is not so for yellow fever. The reason is as follows. Humans are the only host for polio and measles viruses. Consequently, those viruses might be completely eradicated if a sufficient percentage of humans were to comply with vaccination regimens. In contrast, the yellow fever virus infects monkeys that range over thousands of square miles in Africa and the Amazon jungle. Thus, even with massive vaccination of humans, it would be impossible to eliminate the yellow fever virus from the world.
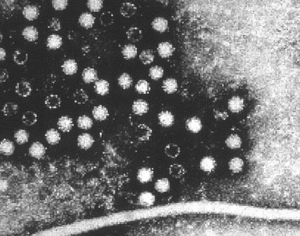
According to the World Health Organization’s estimates, there are still about 200,000 cases of yellow fever per year, resulting in about 30,000 deaths, about 90% of which occur in Africa. The yellow fever virus itself is the prototype virus of the flavivirus family of single-stranded RNA viruses, which also includes dengue hemorrhagic fever virus, Japanese encephalitis virus, and West Nile encephalitis virus, among others.

Yellow fever is somewhat unique among the viral hemorrhagic fevers in that the liver is the major target organ. Consequently, the severe form of yellow fever infection is characterized by hemorrhage of the liver and severe jaundice. But, as in infections caused by other virulent viruses, most cases of yellow fever are mild.
Interestingly, the name “yellow fever” does not have its origin in the yellowing of the skin and eyes that is characteristic of severe disease. Instead, it has its origin in the term “yellow jack,” which refers to the yellow flag that was flown in port to warn approaching ships of the presence of infectious disease.
Yellow fever originated in Africa. It is believed to have been brought to the New World by slave ships in the year 1596. As noted above (and discussed below), yellow fever transmission, from an infected individual or primate to an uninfected one, requires a specific vector, the Aedes aegypti mosquito. The sailing ships of the day inadvertently transported the disease across oceans via the mosquito larvae in their water casks.
Before getting to our stories proper, we note a pair of intriguing instances in which yellow fever profoundly affected New World history. In the first of these, yellow fever was a key factor that led Napoleon to sell the Louisiana Territory to the United States in 1803; an act that doubled the size of the United States. It happened as follows. After Napoleon seized power in France, he reinstated slavery in the French colony of Saint Domingue (now Haiti); doing so for the benefit of the French plantation owners there. In response, the rather remarkable Toussaint Breda (later called Toussaint L’Ouverture, and sometimes the “black Napoleon”) led a slave revolt against the plantation owners. In turn, in February 1802, Napoleon dispatched an expeditionary force of about 65,000 men to Haiti to put down the revolt. The rebellious slaves, many fewer in number than the French, cleverly retreated to the hills, believing that the upcoming yellow fever season would wreak havoc on the French force. And, they were correct. By November 1803, the French lost 50,000 of the original 65,000 men to yellow fever and malaria. Thus, in 1804, Napoleon had to allow Haiti to proclaim its independence, and then become the second republic in the Western Hemisphere. Moreover, there is evidence suggesting that Napoleon’s actual purpose in dispatching the expeditionary force was to secure control of France’s North American holdings. With his expeditionary force decimated by yellow fever and malaria, that was no longer possible and, consequently, Napoleon sold France’s North American holdings (the Louisiana Purchase) to the United States.
 The Louisiana Purchase, in green.
The Louisiana Purchase, in green.
Second, in 1882, France began its attempt to build a canal across the Isthmus of Panama. However, thousands of French workers succumbed to yellow fever, causing France to abandon the project. The United States was able to successfully take up the task in 1904; thanks to the deeds of the individuals in part I of our story, which now begins.
In May 1900, neither the cause of yellow fever, nor its mode of transmission was known. At that time, U.S. Army surgeon, Major Walter Reed, was appointed president of a U.S. Army medical board assigned to study infectious diseases in Cuba, with particular emphasis on yellow fever. Cuba was then thought to be a major source of yellow fever epidemics in the United States; a belief that was said to have been a factor in the American annexation of Cuba.
 Major Walter Reed
Major Walter Reed
When Reed’s board began its inquiry, a prevailing hypothesis was that yellow fever might be caused by the bacterium Bacillus icteroides. However the board was unable to find any evidence in support of that notion.
Another hypothesis, which was advanced by Cuban physician Dr. Carlos Juan Finlay, suggested that whatever the infectious yellow fever agent might be, transmission to humans requires a vector; specifically, the mosquito now known as Aedes aegypti. Reed was sympathetic to this idea because he noticed that people who ministered to yellow fever patients had no increased risk of contracting the disease, which indicated to Reed that people did not pass yellow fever directly from one to another.
Reed, as president of the medical board, is generally given major credit for unraveling the epidemiology of yellow fever. Yet there were other heroes in this story as well. Finlay, whose advice and experience were invaluable to Reed’s board, was one. He was the object of much ridicule for championing the mosquito hypothesis, at a time when there little evidence that might support it. In any case, Reed, in his journal articles and personal correspondences, gave full credit to Finlay for the mosquito hypothesis.
Acting Assistant Surgeon Major James Carroll was another hero. As a member of Reed’s board, Carroll volunteered to be bitten and, promptly, developed yellow fever. Major Jesse Lazear, also a board member, asked Private William Dean if he might be willing to be bitten. Dean consented, and he too contracted yellow fever. Fortunately, Dean and Carroll each recovered. Not so for Lazear. After allowing himself to be bitten, he died after several days of delirium.
Lazear’s contribution to gaining recognition of the mosquito hypothesis went significantly beyond his tragic martyrdom. When Reed examined Lazear’s notebook after his death, Reed found that it contained several key observations. First, Lazear had carefully documented that in order for a mosquito to be infected; it had to bite a yellow fever patient within the first three days of the patient’s illness. Second, twelve days then had to elapse before the virus could reach high enough levels in the insect’s salivary glands to be transmitted to a new victim.
The observations of the board, up to then, convinced Reed and the others that the mosquito hypothesis indeed was correct. Yet Reed knew that more extensive controlled experiments would be needed to convince the medical community. So, he directly supervised those experiments, which involved twenty-four more volunteers, each of whom may rightly be considered a hero.
Just as Reed benefited from Finlay’s insights, William C. Gorgas, Surgeon General of the U.S. Army, applied the findings of Reed’s board to develop vector control measures to combat urban yellow fever; first in Florida, then in Havana, Cuba, and next in Panama, where those measures enabled the United States to complete the canal in 1914. The last urban yellow fever outbreak in the United States occurred in New Orleans in 1905, and the last in the New World occurred in 1999 in Bolivia.
The vector control strategy works for urban yellow fever because the Aedes aegypti mosquitoes have a very short flight range and, consequently, the female mosquito does not stray far from the source of her blood meal before laying her eggs. Thus, it is only necessary to control the vector population in the immediate vicinity of human habitation. In practice, this is accomplished by draining potential mosquito breeding sites such as swamps and ditches, and destroying water-collecting objects such as discarded tires.
After Reed’s board was disbanded, he made yet another key contribution to the wiping out of yellow fever. The focus of the board had been on the means of yellow fever transmission; not with the infectious agent itself. In 1901, at the suggestion of William Welch, an eminent Johns Hopkins pathologist, Reed and James Carroll (who nearly died of yellow fever after being experimentally infected while in Cuba), asked whether yellow fever might be caused by a filterable virus. Indeed, they found that they could infect volunteers by inoculating them with filtered serum taken from yellow fever patients. What’s more, theirs was the very first demonstration of a human illness being caused by a filterable agent. That is, yellow fever was the first human illness shown to be caused by a virus. [Pasteur developed an attenuated rabies vaccine in 1885, more than a decade before the discovery of viruses. Remarkably, this most brilliant of experimentalists did not recognize that he was dealing with a previously unknown, fundamentally distinct type of infectious agent; the topic of a future posting.]
[Aside: Walter Reed spent the early years of his Army career at different posts in the American west. The Mount Vernon Barracks in Alabama, which served as a prison for captured Apache Native Americans, including Geronimo, was a particularly interesting stop for Reed. Captain Walter Reed, serving as post surgeon in the 1880s, looked after Geronimo and his followers.]
Part II of this posting concerns the development of Max Theiler’s yellow fever vaccine. But first, here is a bit more background.
Vector control measures ended yellow fever epidemics in most, but not all urban centers worldwide. Outbreaks have not occurred in the United States for more than a century. However, jungle yellow fever still persists in areas of Sub-Saharan Africa and, to a lesser extent, in tropical South America. Individuals who are infected in the jungle by wild mosquitoes can then carry the virus to densely populated urban areas, where Aedes aegypti mosquitoes can transmit the virus from one individual to another. [Vector-mediated, human-to-human transmission happens because the level of yellow fever virus in the blood of an infected person becomes high enough for the infected person to transmit the virus to a biting mosquito. In this regard, the yellow fever virus is an exception to the generalization that humans are a “dead end” host for arthropod-borne (arbo) viruses.]
Fortunately, people who live in high risk areas for yellow fever can be protected by vaccination. Indeed, the World Health Organization’s strategy for preventing yellow fever epidemics in high risk areas is, first, to mass immunize the population, and then to routinely immunize infants. [Vaccinated American or European visitors to West Africa or the Amazon need not be concerned about yellow fever. However, the risk to an unvaccinated person of acquiring yellow fever during a two-week stay at the height of the transmission season (July through October), is estimated to be 5%. Individuals wanting to enter or return from countries where yellow fever is endemic may need to show a valid certificate of vaccination. ]
Part II of our story, concerning Max Theiler and the development of the yellow fever vaccine now begins.
Even as late as the 1920s, some reputable bacteriologists remained unconvinced by the earlier findings of Reed and Carroll that yellow fever is caused by a filterable agent. Instead, they persisted in the belief that the illness is caused by a bacterium. The notion of a bacterial etiology for yellow fever was finally put to rest after A. H. Mahaffy in 1927 discovered that the yellow fever agent could be propagated and cause illness in Asian rhesus monkeys. With an experimental animal now at hand, yellow fever workers were able to prove conclusively that the disease is caused by a virus. [Mahaffy drew the virus he used in his experiments from a 28-year-old African man named Asibi, who was mildly sick with yellow fever. That isolate, referred to as the Asibi strain, will play an important role later in this anecdote.]
Regardless of the significance of the discovery that the yellow fever virus could be propagated in rhesus monkeys, Max Theiler had to contend with the fact that these monkeys were quite expensive; especially for a not yet established young investigator. [They cost the then princely sum of about $7.00 apiece.] As for mice, while they could be bred for pennies apiece, other researchers were not able infect them via the usual practice of inoculating them under the skin or in the abdomen. However, Theiler took a cue from Pasteur’s inability to propagate the rabies virus in laboratory rabbits until he put the virus directly into their brains. Thus, in 1929 Theiler attempted to do the same with yellow fever virus in mice.
 Max Theiler
Max Theiler
Theiler’s attempts to infect the mice by intracranial injection were a success. All of the inoculated mice died within several days. Surprisingly, the dead mice did not display the liver or renal pathology characteristic of yellow fever. Instead, the mice appeared to have succumbed to inflammation of their brains. Thus, the yellow fever virus appeared to be neurotropic in mice. Also, Theiler himself contracted yellow fever from one of his inoculated mice. He was fortunate to survive.
A fortuitous result of Theiler’s perilous bout with yellow fever was that he had become immune to the virus, as revealed by the presence of antiviral antibodies in his blood. Importantly, Theiler’s acquired immunity to the virus validated the possibility of developing an attenuated yellow fever vaccine. And, in a sense, Theiler was inadvertently the first recipient of the nascent vaccine he soon would be developing.
Theiler also determined that the virus could be passed from one mouse to another. And, while the virus continued to cause encephalitis in mice, it caused yellow fever when inoculated back into monkeys; quite a unique and striking set of findings. But, and crucially significant, while continued passage of the virus in mice led to its increased virulence in those animals, the virus was concurrently losing its virulence in monkeys. [In 1930, Theiler moved from the Harvard University School of Tropical Medicine to the Rockefeller Foundation’s Division of Biological and Medical Research. The Rockefeller Foundation shared facilities with the Rockefeller Institute (now University); although it was otherwise administratively separate from it.]
Since the mouse-passed virus was becoming attenuated in monkeys, Theiler’s belief in the possibility of generating an attenuated yellow fever vaccine was bearing out. However, because the mouse-passed virus remained neurovirulent in mice, Theiler was reluctant to inoculate that virus into humans. In an attempt to solve this problem, Theiler turned from passing the virus in the brains of live mice and, instead, began passing the virus in mouse tissue cultures.
Theiler carried out seventeen different sets of trials to further attenuate the virus. In the 17th of these, Theiler used the wild Asibi strain, isolated earlier by Mahaffy. Initially, this virus was extremely virulent in monkeys, in which it caused severe liver damage. But, after passing the virus from culture to culture several hundred times, over a period of three years, a flask labeled 17D yielded the virus that was to become the famous 17D yellow fever vaccine.
Theiler never gave a satisfactory accounting for the “D” in the “17D” designation, and for what, if anything became of A, B, and C. Regardless, the genesis of 17D was as follows. Theiler initially took an Asibi sample that had been multiplying in mouse embryo tissue and continued passing it in three separate types of minced chicken embryo cultures. One of these sets contained whole minced chicken embryos, and was designated 17D (WC). A second set contained chick embryo brain only, and was designated 17D (CEB). In the third set, the brains and spinal cords were removed from the otherwise whole chick embryo tissue cultures. This set, alone among all the sets, generated an attenuated virus that did not induce encephalitis when injected directly into monkey brains. Indeed, Theiler removed the central nervous systems from the chicken tissue in this set of cultures, in the express hope of generating just such an attenuated virus. And, by hook or by crook, the virus emerging from that particular set of passages became the vaccine that is now known simply as 17D.
Field tests of Theiler’s yellow fever vaccine were underway in 1937 in Brazil, and were successfully completed by 1940. In 1951 Theiler was awarded the Nobel Prize in Physiology or Medicine for developing the vaccine.
Next, we return to a point noted above, and discussed in two earlier postings. Neither Jonas Salk nor Albert Sabin were awarded Nobel prizes for developing their polio vaccines (1). And, Maurice Hilleman was never awarded a Nobel Prize, despite having developed nearly 40 vaccines, including those for measles, mumps, and rubella (2). Indeed, Max Theiler’s Nobel Prize for the yellow fever vaccine was the only Nobel Prize ever awarded for a vaccine! Why was that so?
Alfred Nobel, in his will, specified that the award for Physiology or Medicine shall be for a discovery per se; not for applied research, irrespective of its benefits to humanity. With that criterion in mind, the Nobel committee may have viewed the contributions of Salk and Sabin as derivative, requiring no additional discovery. [Hilleman’s basic discoveries regarding interferon should have been sufficient to earn him the award (2). The slight to him may have been because the Nobel committee was reluctant to give the award to an “industrial” scientist. Hilleman spent the major part of his career at Merck & Co.]
So, what was there about Theiler’s yellow fever vaccine that might be considered a discovery? Hadn’t Pasteur similarly developed an attenuated Rabies vaccine in 1885?
Perhaps the “discovery” was Theiler’s finding that passage of the Asibi strain of yellow fever virus in chick embryo cultures, which were devoid of nervous system tissue, generated attenuated yellow fever virus that was no longer neurovirulent in mice and monkeys. But, consider the following.
Theiler indeed believed that removing the brains and spinal cords from the chick embryo cultures in which 17D had been serially passed was the reason why the virus lost its neurovirulence. Nevertheless, as a serious scientist he needed to confirm this for himself. So, he repeated the long series of viral passages under the same conditions as before. But, this time, there was no loss of neurovirulence. Thus, a cause and effect relationship, between the absence of the brains and spinal cords from the tissue cultures and the emergence of non-neurovirulent virus, was not confirmed.
So, perhaps the Nobel committee merely paid lip service to the directives in Alfred Nobel’s will. In any case, Theiler’s 17D yellow fever vaccine has had a virtually unblemished safety record, and is regarded as one of the safest and most effective live-attenuated viral vaccines ever developed.
Theiler’s unshared 1951 Nobel award paid him $32,000. At the time, he resided in Hastings-on-Hudson; a village in Westchester County, NY, from which he commuted to the Rockefeller labs. Theiler’s next door neighbor in Hastings-on-Hudson was Alvin Dark, the star shortstop of the New York Giants. Nobel laureate Max Theiler was known to fellow commuters from Hastings-on-Hudson as the man who lives next door to Alvin Dark.
Virus Hunters, by Greer Williams (Alfred A, Knoff, 1960) was my major source for the material on Max Theiler.
1. Jonas Salk and Albert Sabin: One of the Great Rivalries of Medical Science. On the blog.
2. Maurice Hilleman: Unsung Giant of Vaccinology. On the blog.